Which Therapist: Factors To Consider

Choosing a suitable health professional can be time consuming and also very expensive, especially if after getting ‘treated’ the pain returns. To make things worse, the difference between a physiotherapist, sports therapist or sports massage therapist is often not clear. How about an osteopath, chiropractor or podiatrist? Who should runners be going to?
Resolving running related injury/pain is not black and white but there are certain guidelines that could help you minimise frustration and increase the chances of receiving effective therapy. In today’s world, there is considerable overlap between the different professions offering their services for runners. This has largely been the product of a shift away from traditional ideology towards more rational, scientific explanation and a systematized approach to managing injury.
Recognising the role of not just physical structure to pain but also psychological and social influences means that most health professionals now understand (or at least should understand) the importance of focussing attention on the person rather than just the injury. I say ‘should’ because although many health professionals across all disciplines have successfully evolved in order to integrate their treatment into modern science based practice, some have evolved more than others.
Chiropractic
Chiropractic is a good example of a discipline that has had to evolve. Founded in the late 19th century, it flourished in a world where the concept of medical trials and evidence based practice was unheard of. The modern day practice of having a chiropractor ‘realign’ your spine stems from Chiropractic founder Daniel David Palmer of Iowa. Palmer believed that poor health was due to slight misalignments in the spine, which he referred to as ‘subluxations’. His theory was that these misalignments interfered with the flow of a ‘life force’ he called ‘innate energy’ and that by performing ‘adjustments’ he could restore free flow of this life force from the brain to the tissues.
It will hopefully come as no surprise to you that there is absolutely no scientific evidence for the existence of Palmer’s ‘subluxations’ or ‘innate energy’ and despite his promises that chiropractic adjustment could cure 95% of all diseases, studies have failed to that show that they can cure any disease; some research suggests that chiropractic adjustment can provide benefit for back pain but most people agree it’s probably not down to the ‘restoring of life force’.
So what do we take from this example? Should we all stop seeing chiropractors? No, that’s not my message at all. Many chiropractors today realise the limitations of their founder’s original philosophy and have added therapeutic physical rehabilitation to their services in order to integrate their treatment better within the medical system. These chiropractors are referred to in the trade as ‘mixers’. However, other chiropractors (referred to as ‘straights’) have refused to budge from the original teachings and continue to believe (and sell) the idea that adjustments can cure headaches, period pains, ear infections, infantile colic, asthma, allergies, digestive disorders, and more. Should you seek the services of a ‘straight’ Chiropractor to help you with your running related injury? I’ll leave that for you to decide.
“Many chiropractors today realise the limitations of their founder’s original philosophy and have added therapeutic physical rehabilitation to their services in order to integrate their treatment better within the medical system.”
Osteopathy
Despite being regarded by many as a more modern discipline, osteopathy is actually slightly older than chiropractic. It is suggested that its founder Andrew Taylor Still had a strong influence on Palmer’s ideas of chiropractic. Andrew Taylor Still believed that many of the conventional medical practices of his day were causing more harm than good and proposed that disease and physiologic dysfunction were the product of a disordered musculoskeletal system. He argues that bone (the ‘osteon’) was the starting point from which one could ascertain the cause of many pathological conditions and that manipulating joints (not just the spine) physicians could treat a variety of diseases and spare patients the negative side-effects of drugs. He opened the American School of Osteopathy in Kirksville, Missouri in 1892.
As is the case with Chiropractic, the idea that manipulating a joint can cure diseases has as yet not been proved scientifically. Many osteopaths have therefore likewise moved on from their founder’s original beliefs, with the profession splitting into two clear branches: manual medicine osteopaths (non-physician) and osteopathic physicians (full scope of medical practice – D.O.s in the United States). The former (referred to as just Osteopaths in Europe) have a scope of practice that excludes most medical therapies and relies more on the original manipulative medicine and alternative medical modalities introduced by Still.
As in the case of chiropractic adjustments, there is evidence that osteopathy can help reduce lower back pain and some evidence to suggest it may also be effective for some types of neck, shoulder or lower limb pain. However, there is no evidence that osteopathy is effective as a treatment for the often advertised headaches, migraines, painful periods, digestive disorders, depression and excessive crying in babies (colic).
As with Chiropractors, the type of treatment and advice you receive can vary considerably depending on the beliefs of the osteopath you visit. I have worked with some exceptional osteopaths whose ability to consider the whole body as opposed to just the injury has allowed them to help many of the runners I refer to them. But then we have cranial osteopaths who believe their hands can detect a craniosacral ‘rhythm’ in your cranium (skull bones) and that by manipulating your skull they can relieve disease (including cancer).
Looking at the science, the skull does not consist of moveable parts and the only ‘rhythm’ detectable is related to the cardiovascular system. Studies show that craniosacral osteopaths have been unable to consistently come up with the same measurements of the alleged ‘rhythm’. Would you want to place yourself in the hands of someone who believes they can move skull bones and detect body rhythms? Again, the choice is obviously yours but the take home message is type of treatment can differ from one osteopath to another, just as it can with chiropractors.
“As is the case with Chiropractic, the idea that manipulating a joint can cure diseases has as yet not been proved scientifically. Many osteopaths have therefore likewise moved on from their founder’s original beliefs.”
Physiotherapy
Physiotherapy has its origins in massage, manipulation, and exercise, as practiced by Per Henrik Ling, the ‘Father of Swedish Gymnastics’. His methods of rehabilitation encouraged four nurses in Great Britain to form the Chartered Society of Physiotherapy in 1884, followed by The School of Physiotherapy in New Zealand in 1913. The first School of Physiotherapy (physical therapy) in the United States was established at Walter Reed Army Hospital in Washington D.C. following the outbreak of World War I.
An important distinction between the roots of Physiotherapy and those of other health care professions is that it was catalyzed by research. Manipulative procedures to the spine and extremity joints similar to those seen in chiropractic and osteopathy were still used but as part of a much larger treatment plan including exercise, massage, and traction. The foundational thrust towards a scientific approach means that physiotherapy has had to evolve less than its counterparts, but has still nevertheless had to evolve as our understanding of the human body and mind develops.
Sports Therapy
Since the 1980’s, Sports Therapy has presented itself as a discipline specifically concerned with the prevention of injury and rehabilitation of the sports related patient. Though the full scope of learning to qualify as a Sports Therapist is less than that of a physiotherapist (a protected title that requires appropriate university education), Sports Therapy utilises many of the principles of sport and exercise science from physiotherapy and therefore presents considerable overlap. There is no guarantee that a physiotherapist will be able to help you more than a Sports Therapist.
As with all of the professions we have looked at, the key component is therapists pursuing ‘continuing professional development’ (CPD) in order to stay up to date with modern evidence based practice.the brain and nervous system is not just a case of saying ‘pull yourself together’ or ‘chill out’ (although that can help); it’s about progressively challenging your system to suitable exercise load so that the threat is gradually removed and sensitivity thresholds return to ‘normal’ levels. This is one of the primary goals of effective rehabilitation and the medical professional you see needs to be aware of this.
Five Ways To Select A Health Professional
The point of this article is to show that it’s not as simple as choosing chiropractors for bony issues, physiotherapists or sports therapists for muscular pain, or osteopaths for anything in the middle. The quality of treatment and advice you receive can vary considerably between practitioners of the same discipline. I cast no doubts on any one profession.
The need to evolve means that you can find good and bad in all professions and there are certainly more options out there than I have covered in this article. My best advice would be to find a health professional who ticks all of the boxes below and hold on to them. Whatever their discipline, let them be your ‘go-to-therapist’ for all running related injury advice as they will then be able to refer you to an alternative specialist if they feel your needs fall outside of their personal skill set.
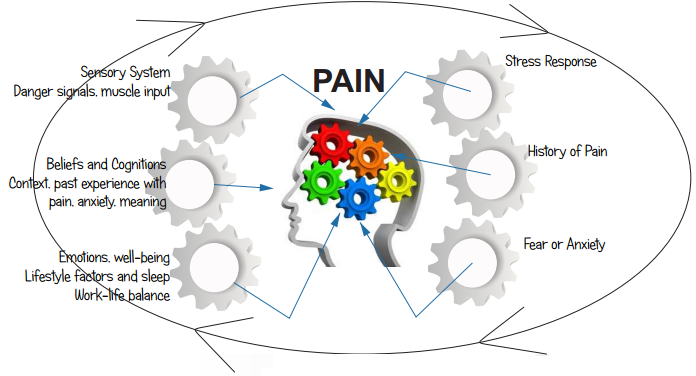
Health professionals up to date with the latest research will (if asked) explain to you that pain is not solely the product of damaged tissue. If pain depended on the presence of damaged tissue, how is it that somebody who had their leg amputated years ago still feels pain in their no longer existing foot? How is it that we can wake up one morning with a bruise but have no recollection of how it got there? Why do we sometimes only realise we are injured when we see the blood? The answers lie in modern concepts from pain science that teach us pain is an output of the brain in reaction to a perceived threat, and is not dependent on actual tissue damage.
Though a leg has been amputated, the brain still has cognitive and emotional memories of that leg (every body part has its own ‘cortical map’) meaning that as far as the brain is concerned that leg still exists, and if threatened by a past memory or fear of danger it will output a pain that you will ‘feel’ in that body part (phantom limb pain). Likewise, if you are having a great time at a party or you are busy trying to control your kids in a supermarket, your brain may see no priority in letting you know that you have just banged your leg on a table, so you wake up the next day with a nasty bruise but no memory of how.
If you go to a health professional with a painful knee and they focus solely on ‘fixing’ that knee, there is a danger that they will miss many other factors that could be contributing to your pain. This is even more significant if the pain you are suffering from has been going on for a long time (persistent or chronic) because although your tissues have healed, your brain may still see the action of running as a threat, and therefore output pain when provoked. No one is saying the pain is all in your imagination – all pain is very real.
“Find a health professional who ticks all of the boxes. Let them be your ‘go-to-therapist’ for all running related injury advice as they will then be able to refer you to an alternative specialist if they feel your needs fall outside of their personal skill set.”
What we are saying is that in dealing with pain we have to take into account how sensitized your nervous system is, because oversensitivity (e.g. through stress, fear, worry, anger, lack of sleep, etc.) means your brain will be quicker to output pain if you try to run again. Reducing sensitization of the brain and nervous system is not just a case of saying ‘pull yourself together’ or ‘chill out’ (although that can help); it’s about progressively challenging your system to suitable exercise load so that the threat is gradually removed and sensitivity thresholds return to ‘normal’ levels. This is one of the primary goals of effective rehabilitation and the medical professional you see needs to be aware of this.
2. Avoid any treatment that causes considerable pain
Many manual therapists were taught and still believe that they have the power to forcefully ‘break down’ adhesions or scar tissue. They will tell you that to ‘get rid of your knots’ they will need to apply a lot of pressure, so many runners close their eyes and put up with considerable pain in the belief that it is a necessary evil to get ‘fixed’. The reality is different; surgeons use scalpels to cut through scar tissue. It is highly unlikely that any human being has sufficient strength to forcefully change the structure of tissue. Research has shown for example that to produce just a 1% deformation in fascia (the structure that makes up the IT band) a therapist would need a force greater than that of a lion’s jaw. A crocodile could get through fascia, but a therapist’s elbow… no.
Up to date health professionals realise that massage probably works by relaxing the nervous system, which in response stops outputting pain and relaxes the tension in muscles. A health professional who understands the ‘how’ will therefore tend to avoid doing anything that generates too much pain as this could agitate the nervous system further and in all probability cause more pain down the line. Ensuring the runner on the couch is relaxed during a treatment is very important to the modern day medical professional.
Ever been told your hip pain is because your legs are different lengths? Your neck pain is because you have one shoulder higher than the other? Lower back pain because your pelvis is tilted too far forwards? Sadly, none of these explanations for pain are evidence based. They are the product of traditional therapy schools based around the pursuit of ‘alignment’, with the idea that if you are ‘symmetrical’ you will be pain free.
Research has fairly conclusively proved no clear link between asymmetry and pain: there are plenty of asymmetrical runners with one shoulder slightly higher than the other, one leg slightly longer, who are not in pain; likewise, there are runners who are totally symmetrical but are in pain. There are very few ‘norms’ when you look at human anatomy. It is extremely difficult (if not impossible) to blame pain on structural ‘misalignment’ or ‘asymmetry’ and any health professional that continues to do so probably needs to update their knowledge base.
Health professionals up to date with the latest research will also realise that although there are a variety of tools they can use which will help you leave the appointment feeling less pain and moving more freely, these effects are generally short term and must be regarded as only one part of the overall rehabilitation plan. Long term changes to pain and movement rely on you taking control, modifying activity as necessary and most importantly doing your exercises.
One of the biggest complaints voiced by medical professionals is that runners do not do the rehab exercises they were given, but quite often the reason for that is that their importance was not stressed sufficiently. If a health professional is not giving you homework (with clear time goals and weighted progressions), you may well be missing out on an important part of your rehabilitation.
“Research has fairly conclusively proved no clear link between asymmetry and pain: there are plenty of asymmetrical runners with one shoulder slightly higher than the other, one leg slightly longer, who are not in pain.”
With such a high incidence of running related injury, there is naturally an ample supply of dubious ‘quick fixes’ and ‘magic bullets’ to cure all. When searching for the latest way to push ourselves to the limit without succumbing to injury, the adverts on social media (Facebook is an absolute goldmine) can come across as very tempting and persuasive. Injury ‘prevention’ is probably impossible (especially as science has still yet to discover what causes a lot of running injuries).
What we can do is try and reduce how often injury occurs by following sensible, and where possible evidence backed advice. When seeking help from a medical professional, watch out for scientific sounding promises and far reaching claims. Anybody offering a ‘one-size-fits-all’ fix for any runner is likely to be a more skilled business person rather than therapist.
As far as special products & techniques designed to manage or prevent running injuries goes, there is not a lot that has not already been done. New trends tend to be old ideas re-dressed to look like the latest evidence, and if they have had to be re-dressed, chances are they were never evidence based in the first place. Such adverts work by offering runners what they want (a quick fix) as opposed to what they need. Just because a medical professional is successful promoting themselves in social media does not mean they will be successful in helping you as a runner. That said, if you have seen a health professional for more than four sessions and seen no improvement, it may well be worth moving on!
In Summary
Ten years ago, my top recommendations for choosing a health professional would have been (a).Check their qualification (b).Make sure they have running experience. The latter is obviously still an advantage, but only if they are up to date and understand that what works for them will not necessarily work for you. Modern understanding of pain and injury means that traditional certificates are no longer a guarantee of effective treatment.
As we have seen above, many of the treatment modalities still offered by recognised professions have no scientific backing and could be a waste of your time and money. When they do seem to work, you have to consider the possibility that your injury just got better of its own accord, especially if you’ve been seeing that health professional for four weeks or more.
Choosing a health professional who cares about ‘how’ a treatment works (if you know how something works, you are more likely to be able to make it work better) and endeavours on a daily basis to critique their own discipline in pursuit of using as much evidence based practice as possible is probably the best way you can find a health professional you can trust.
Have you had any interesting experiences seeing different types of health professionals? Maybe you are a health professional yourself and would like to pick up on something in the article? Feel free to use the comments section below!
Related Posts
How to Breathe when Running
The question of ‘how to breathe when running’ is one that many runners find themselves pondering, especially those new to running or starting to experiment with more intense sessions like sprint or hill intervals. Should we breathe through the mouth or nose? Is there a particular rhythm or technique we should be using?
Post Run Stretching – Try Some HELP.
Does post run stretching help reduce soreness or reduce risk of future injury? The research says no, but you could try some H.E.L.P.
Cadence Testing Brighton Marathon
Cadence when running refers to how many times the feet touch the ground per minute. Some schools of running suggest all runners shoud run at the same cadence, but is this supported ny research? Can reducing or increasing cadence help reduce running injury and increase performance?





0 Comments